
California
can not begin to solve its structural budget deficit problem without first
addressing the fundamental issues of health care’s structure and cost.
It’s
Time for Fundamental Health Care Reform
By David J. Gibson, MD
|
|
California
can not begin to solve its structural budget deficit problem without first
addressing the fundamental issues of health care’s structure and cost. |
 A consensus is forming.
California can not begin to solve its structural budget deficit problem
without first addressing the fundamental issues of health care’s structure and
cost. For years we have been avoiding the need for a substantive policy debate
by concentrating our attention upon how we should pay for the current system.
Further debates over single payer vs. private health plans will not lead
to a resolution of California’s structural budget deficit problem.
The longer we delay in joining this debate, the more likely it will be
that California’s budgeting process will continue to spiral out of control and
will ultimately lead to the State’s insolvency.
A consensus is forming.
California can not begin to solve its structural budget deficit problem
without first addressing the fundamental issues of health care’s structure and
cost. For years we have been avoiding the need for a substantive policy debate
by concentrating our attention upon how we should pay for the current system.
Further debates over single payer vs. private health plans will not lead
to a resolution of California’s structural budget deficit problem.
The longer we delay in joining this debate, the more likely it will be
that California’s budgeting process will continue to spiral out of control and
will ultimately lead to the State’s insolvency.
The
cost trend indicator warnings have been sounding for some time.
Health expenditures per person rose 32% between 2000 and 2004 and
continue to outpace the rest of the economy. The accompanying graph illustrates
the crushing burden America’s health care system places upon the economy.
By 2013, health care expenditures are expected to double, with an
estimated 18% of the domestic economy devoted to healthcare.
In 2004, Medicaid cost the
states and the federal government more than $300 billion.
This year the program is projected to cost the federal government alone
over $190 billion with the combined state and federal
projected expenditure to be roughly double this number.
According to the National
Assn. of State Budget Officers, spending on Medicaid grows by around 8% a year
on average, while total state spending grows an average of 4.5%.
This growth is outpacing state revenues and is now a larger component of
total state spending than elementary and secondary education combined.
This program alone is driving most of the states toward insolvency. Complicating the state’s Medicaid problem, the federal
government is indicating that it will likely lower the federal contribution to
the program next year in its drive to reduce deficit spending.
The public is becoming aware
that the above trends are not sustainable.
As a result, we are now hearing calls from across the political spectrum
a call for “fundamental” change in health care; but, before we begin
discussing fundamental changes within the health care system, it would serve us
well to examine what this change will involve.
The
current system’s structure
We should begin this
discussion by understanding that health care’s cost structure is based upon an
artificially constructed market foundation. What we now have in America is a
pricing structure for health care that is based upon the best funded payer’s
ability to pay (the employer and the government) rather than what patients and
their families can ever afford. This
has produced inflationary trends that are completely independent of the market
forces that discipline the rest of America’s economy.
We also have an acuity based
health care system that spends most of its resources in the last two weeks of
life. In essence, we try to use medicine to defeat death. Of course, this does
not work.
Both of the above realities
define our current health care system and represent an irrational foundation for
America to have used in building its current health care system.
As we begin this process of
examining fundamental changes, we must not confuse the terms fundamental with
incremental. Getting something of value in return for concessions in a
negotiated framework will not work. “Fundamental” reform requires focusing
on the patient and his or her needs — not what benefits those making money in
the current system will continue to exploit.
The primary inflation drivers
in health care are illustrated in the accompanying graph[1]
and include hospitals, pharmaceutical manufacturers, health insurance companies
and the cost of labor. These are the areas where fundamental reform needs to
begin in the industry. Reform outside the industry such as unfunded mandates by
the legislature and America’s tort system will be required as well but will
not be examined in this article.
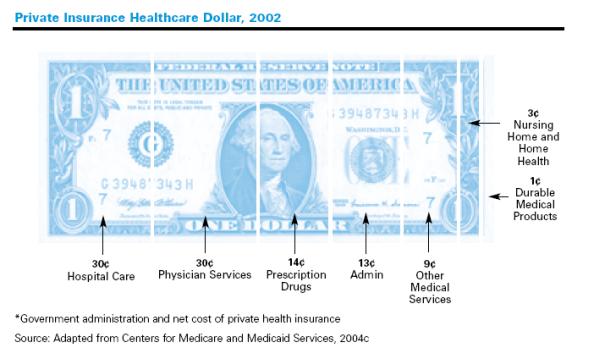
Hospitals
More than half of the
increase in private insurance spending has been driven by outpatient and
inpatient hospital cost. Outpatient costs were the single largest contributor to
increasing premiums in over the past several years.
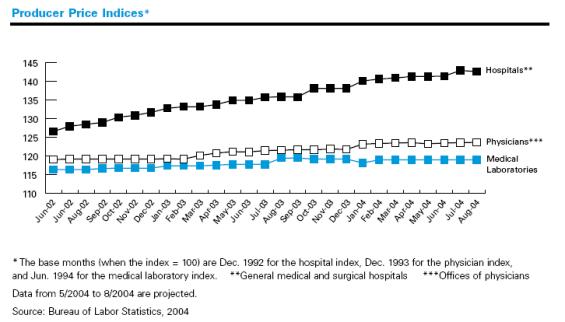
While prices for physician and laboratory services rose about 2%-4% from
June 2002 through August 2004, hospital prices rose 13%.
The following graph[2]
illustrates this relative cost trend.
As we evaluate the role of
the hospital in the evolving health care system, we need to revisit the outdated
idea of isolating the sick and dying from the community. This concept originated
in medieval times to protect society from the sick. This paradigm simply does not translate into the era
of antibiotics.
For starters, it is a foreign
concept. America’s commitment to
an individual’s freedom makes it averse to the very concept of custody.
Taking custody of an individual is the most costly and least productive
of options for treating the sick and dying. In that technology is driving health
care to the ambulatory setting, the system should be designed with less
dependence on institutional care in the future.
Transitioning from an
inpatient, acuity-oriented system to an ambulatory-based system will require
focusing upon these policy issues:
·
Deconstruct
regional hospital oligopolies. It was a major policy
mistake, made by the federal courts over the objection of the Clinton
Administration, to let hospitals coalesce into dominant regional corporations.
More than half of the nation's hospitals belong to larger health-care systems.
Recent studies demonstrate that consumers are disadvantaged in that these
systems drive increased cost to the consumer.[3]
Northern California is dominated by two of these regional systems (Sutter
and CHW) and has some of the highest health care costs in the western United
States as a direct result. These oligopolies should be dissolved.
·
Make
rural hospital monopolies public utilities. In communities with only one
hospital (Marysville, Crescent City, etc.), the hospital should be regulated as
a utility and managed as such. In a utility paradigm, the hospital would be
required to get permission from the people it serves to set charges. These
hospitals now prey on their local communities and destroy rural economies.
·
Prevent
hospitals from expanding into the ambulatory market. Over
the past two decades, hospitals have used the most expensive resource in health
care, their inpatient bed, to leverage contract advantages with managed care
companies. In exchange for inpatient bed discounts, hospitals have been able to
gain a dominant position in the delivery of ambulatory diagnostic and
interventional services (outpatient surgery center and radiation units, etc.).
They have brought their high overhead, monopolistic management style into this
setting and stifled innovation while exacerbating the inflationary problem in
health care. Hospitals should not be allowed to provide services in the
ambulatory market. Furthermore, managed care companies should be prohibited from
linking inpatient discounts with preferred outpatient diagnostic and
interventional contracts.
·
Prohibit
hospital-affiliated doctor groups.
Permitting
hospitals to develop affiliated medical groups was also a public policy error.
Affiliated groups align the physician’s business interests with the hospital
in the latter’s never-ending battle with health insurance companies.
The cacophony of battle between Sutter and Blue Shield (representing
CalPERS) speaks to this issue. A physician’s loyalty represents a long term
commitment to his or her patient and far transcends annual contract
negotiations. Physicians should immediately disassociate their medical groups
from hospitals.
·
Break
up the Emergency Room monopoly. Hospitals and ER medical groups have
leveraged their contract position with third party payers so that professional
fees for similar services are marked up by a factor of three over all other
alternatives in the ambulatory setting. Furthermore, the hospital marks up
supplies such as pharmaceuticals by a factor of ten or considerably more.
Stacking the reimbursement system in such a distorted way makes the ER the only
option after hours or on weekends. There is no incentive for physicians to
create cost effective after hours alternatives. These disproportionate
reimbursement structures should be eliminated.
·
Make
hospitals participate in the safety net for the poor, or pay taxes.
Not-for-profit
hospitals should rediscover their only
mission – to care for the poor. Not-for-profits
were not designed to compete in the for-profit market. Spending on a technology
arms race and pouring money into advertising is a diversion from their
fundamental mission. Complaints by non-profit corporations over their safety net
responsibilities are unseemly.
Another health care player
reporting record earnings is the health insurance industry. Underwriting health
care is, at best, a minor peripheral activity for these companies. Most of their
activity is focused upon intermediation of health care transactions. There are
far more efficient alternatives in the market today.
Perhaps the most insidious
effect of managed care has been the insurance company development of discounted
provider networks. These networks
now disadvantage the individual patient who pays cash. This disadvantage
translates into a fiscally dangerous environment for the 44 million Americans
without health insurance as they confront the health care system.
This discount structure is
counterintuitive. No other sector of our economy marks up fees for cash customers. In addition, these networks reward the
status quo, guarantee hospital hegemony and inhibit any incentive to innovate.
Health insurance companies
have no other core competency outside these networks. Their adjudication of
claims and financial intermediation of services use analog technology discarded
by the financial services industry two decades ago. This outdated technology has
inhibited the deployment of digital technology in health care.
Health insurance companies
have utterly failed as intermediaries. On their watch, inflationary trends in
the industry have been well above all other segments of the economy.
Eliminating insurers as
intermediaries in health care would be a positive outcome in a new fundamentally
restructured health care system.
Prescription
drugs and hospital outpatient costs have been the fastest growing components of
privately funded healthcare costs for the past decade.
For this reason alone, pharmaceutical costs and industry structure can
not be omitted when health care reform is implemented.
As we open this subject, it
is important to understand that the core competency of pharmaceutical companies
is not research, but marketing. The debate over stem cell research illustrates
this. There is no ban on privately-funded stem cell research anywhere
in America. There is a restriction on federal funding for some of its
components.
If they chose to do so,
pharmaceutical companies could devote unlimited amounts of basic research to
stem cells. Of course, they have not done so in the past and will not in the
future.
Dr. Marcia Angell, the former
editor of the New England Journal of
Medicine, has documented[4] that most of the current
pharmaceutical breakthrough products on the market were developed from basic
research funded by the National Institutes of Health in academic centers.
Pharmaceutical companies then appropriated these publicly funded research
efforts and brought products to the market under exclusive patent protections.
The marketing emphasis in
pharmaceutical companies is evident by where they do invest their resources.
Marketing expenditures of the drug industry
have been estimated at $12 billion to $15 billion every year, or about $8,000 to
$15,000 per physician. There are
nearly 90,000 drug company salesmen in the United States, about one salesperson
for every 4.7 office-based physicians. A
2001 survey found that an estimated 92 percent of doctors received free drug
samples from companies; 61 percent received meals, tickets to entertainment
events, or free travel; and 12 percent received financial incentives to
participate in clinical trials.[5]
It is now becoming evident
that the pharmaceutical industry is morphing into an entirely new structure.
This transition is traumatic for the pharmaceutical industry. As a result, there
is great harm now being inflicted upon health care as old pharmaceutical
companies resist change.
All the large manufacturers
have business models built on delivering “block buster” products to the
market. Block buster products target common health problems and are prescribed
by generalist physicians. Examples include: Proton Pump Inhibitors (PPI) for
gastrointestinal ulceration; Selective Serotonin
Re-uptake Inhibitors (SSRI) for
depression; and HMG-CoA (3-hydroxy-3-methylglutaryl coenzyme A) reductase
inhibitors, referred to as Statin products for hypercholesterolemia.
Most of these “low hanging
fruit” products have been introduced to the market and either have, or soon
will, lose patent protection. The current pipeline for new products is
inadequate to sustain the pharmaceutical companies and investors are reacting.
In late 1998, pharmaceutical stocks traded at 40 times their expected earnings
for the following 12 months. Today,
these stocks trade at less than 14 times their expected earnings, the cheapest
level in eight years. It is clear
that an era is passing. This
situation is analogous to Pan American Airlines which no longer flies chiefly
because its business model did not translate into a fundamentally changed
airline market.
These
multinational pharmaceutical companies are now consolidating while they
compensate for their pipeline deficiencies by marketing “me
too” products. They are also modifying previously introduced products that are
losing patent protection with minor molecular modifications. This strategy
isn’t working.
In
reality, these companies are failing because they lost their ability to
innovate. Over the next decade, most of these old companies will either
disappear or morph into delivering high-margin, lifestyle-enhancing drugs such
as Viagra or Propecia to the market.
The truly innovative new
products coming to market are being developed by small new companies that
generate “orphan” drugs. These products serve only a small number of
patients and are generally prescribed by specialists. Most of the
biologic-produced products, such as Remicade, Enbrel and Humira,
fit into this category. All of the genetic targeted and derived products will as
well. Block buster business models will not deliver these new products at
affordable prices.
The
sooner these older block buster-based companies give way to new companies with
new business models, the better it will be for health care. Society has
entrusted physicians with the exclusive responsibility for prescribing, and it
is incumbent upon us to not allow these older companies to inflict further
damage on America’s health care system as they fail.
Any physician prescribing a
brand product over a generic without head-to-head proof of its superiority,
documented in a national peer-reviewed journal, is doing a disservice to his or
her patient and to America’s health care system.
Resonating through all of
these issues is the reality that the cost of labor in health care is too high.
Before the advent of third-party payers, America’s health care system relied
on the patient and his or her family to pay their health care bills. There was
no inflation problem in health care when the patient paid the bill. Consumers
policed costs far more effectively than have third parties under the current
system.
Paul Starr in his book, The
Social Transformation of American Medicine, documents that doctors
throughout American history have traditionally had meager incomes. In fact,
doctor incomes were roughly commensurate with a school teacher prior to the
advent of third-party payment. The rest of the labor components in the system
were structured proportionately.
As America’s health care
financing system moves away from first dollar coverage and toward higher
front-end payments by patients, most families cannot afford a labor cost
structure that is out of line with the society it seeks to serve.
So, how do we realign the
labor cost structure in health care? We should start with professional licensure
laws. These laws provide one of the primary supports for today’s bloated labor
cost structure in health care.
Professional licensure was
originally developed to protect the patient. It no longer serves that purpose.
Licensure now insulates labor in health care from competition and inhibits
innovation. This is featherbedding at the expense of the patient. It restricts
the availability of culturally and ethnically suited support for the patients in
our evolving society.
Today, the only real purpose
of license defined scope-of-practice is to raise money for politicians. Each
year doctors fight with dentists before the Legislature over how far into the
neck the latter can treat. The same goes for doctors and podiatrists — how far
up the lower leg can the latter go? Defining clinical competence through the
political process is nonsense.
It is no secrete that the
Legislature holds annual “juice sessions” to exploit these
inter-professional conflicts and thereby raise campaign money. This is obscene.
The process serves no useful purpose and should be stopped.
In short, the entire purpose
of licensure and scope-of-practice needs a thorough re-evaluation from the
perspective of what is good for the patient rather than what serves the
interests of the labor force in health care.
It is time to get serious
about “fundamentally” reforming health care. Not doing so will only
perpetuate our self-created culture of delusion. Health care’s inflationary trends will destroy the
financial structure for the State of California in that these trends are not
sustainable. All of organized
labor’s valued private health plans will also be swept away as health care’s
cost trends demand more and more limited resources. In reality, policy makers have no alternative.
They must reform the health care system in the near future.
We can no longer perpetuate
an acuity-based system whose foundation is built upon outdated custodial
institutions. We can no long permit health insurance contracts to warp the
incentives in health care and stifle innovation. We dare not let failing pharmaceutical companies inflict
further damage and we cannot accomplish any of this without bringing health
care’s labor cost structure into line with the rest of our economy.
We have learned that the
system can not be reformed from within. The
players within health care will always opt for more funding rather than reform.
Unfortunately, there is no end to the more funding option.
If 18% of the GDP by 2013 does not adequately fund health care how much
will the industry demand. Will 25%
suffice? How about 50%? Of course we could not educate our children or defend the
country. We live in an era where
health care must co-exist with the rest of America’s economy.
Clearly waiting for internal reform is folly.
We need to devolve
America’s health care system into a less complex and costly structure that
patients and their families can understand and actually pay for. In reality,
there is no choice. Without truly fundamental reforms, our economy cannot
sustain the inflationary juggernaut we have unleashed.
DJGibson@illuminationmedical.com
[2]
ibid
[3]
Health Affairs, Vol 24, Issue 1, 213-219
[4]
“The Truth About the Drug Companies;” M. Angell; Random House; ISBN
0-375-50846-5
[5]
Doctors
and Drug Companies;
David Blumenthal; NEJM; Volume 351:1885-1890; Number 18. http://content.nejm.org/cgi/content/extract/351/18/1885